Dutch researchers discover how coronavirus affects some people more than others
In the race to vaccinate people across the globe, researchers from Amsterdam have cracked the code that explains one of the most troublesome symptoms of COVID-19. And through international collaboration, they have potentially made a breakthrough in treating the disease with an already approved drug.
Shortness of breath is one of the main symptoms caused by the novel coronavirus. It shows there is an underlying issue specifically targeting the lungs. Although ICU admissions only make up a small percentage of COVID-19 cases, ICUs around the world have filled up due to an inflammation in the lungs. Scientists at Amsterdam UMC have developed a more in-depth understanding of how the virus affects the lungs.
What we know now is that COVID-19, the disease that is produced by the novel coronavirus, mainly targets the lungs. This has been confirmed worldwide by pulmonologists, doctors specialised in the respiratory system. A team of researchers from Amsterdam UMC decided to focus their attention to better understand the effects of the virus on the lungs.
“We discovered why some people get mild disease while others get really sick. Apparently it is due to the reaction of the immune cells to the antibodies,” said Jeroen Den Dunnen, one of the researchers leading the discovery.
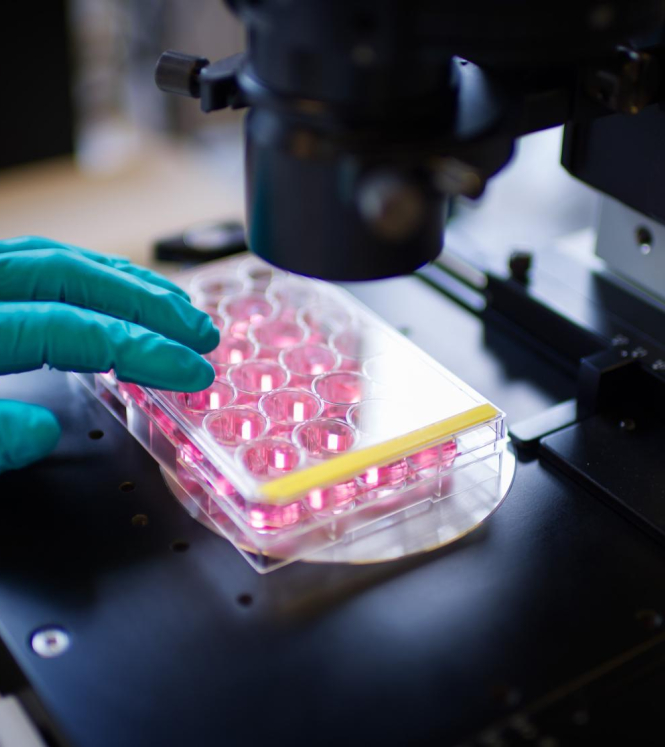
After reviewing previous coronaviruses like SARS, Jeroen den Dunnen, along with his colleague Professor Menno de Winther, decided to look more closely at the behaviour of the human antibodies. They extracted antibodies through blood samples from patients who had suffered mild and severe cases of COVID-19. The spike protein, a protein part of the virus which allows interaction with human (and animal) cells, was added to the antibodies in laboratory petri dishes.
The researchers then observed how the antibodies latched onto the spike protein. What they then figured out was “the molecular mechanism” explained Den Dunnen and De Winther. When the immune cells were released into the dishes with the spike protein, an immense inflammatory reaction took place. What’s interesting is that it only occurred in patients who had suffered a severe case of COVID-19, who naturally would have “produced more antibodies than those who suffered a mild case of the infection.”
The discovery didn’t stop there. Not only did the patients with severe cases produce more antibodies, they also produced antibodies with a different shape. This combination resulted in damage to the blood vessels located in the lungs. This then produced a build-up of fluid and protein, causing severe tissue damage. This damage explained what we were all witnessed in severe COVID-19 patients: a shortness of breath and in extreme cases, blood clots blocking blood vessels. The study was funded by ZonMw and published recently in Science Translational Medicine.
International collaborative efforts paying off
With different vaccines being approved and used around the world, a return to normal life seems within reach. However, Den Dunnen and De Winther explained that treating the current severe cases of coronavirus is still the main priority as mutations will continue to surface around us. The next step for the researchers was then to figure out how to treat the inflammation caused by the antibodies.
The researchers explained that they knew they needed to “find a treatment that would make those immune cells insensitive to the antibodies without taking away the good antibodies. We hypothesised that a drug would work,” Den Dunnen and De Winther said.
The researchers discovered a likely contender in an existing approved drug. Last year, the European Medicines Agency approved Fostamatinib, often referred to as Tavlesse, to be used for auto-immune conditions. Working together with the National Institutes of Health (NIH) in America, the first results are promising. Patients who received the drug recovered faster than those who received a placebo alternative. However, researchers say the sample size was too small to draw any definitive conclusions. By August, a phase 3 trial by the NIH of more than 300 patients in 42 hospitals across the American continents should give more insight.
Den Dunnen and De Winther told us that when your body is faced with a viral infection, we often blame the virus. However, we now know that it’s actually our immune response that is causing trouble. The answer, according to the Dutch researchers, is to “knock down the immune system. But not completely, because then you have no defense against the virus”. With future coronaviruses likely becoming pandemics, drugs like Fostamatinib prove very beneficial as they target the immune response specifically, without throwing our whole body into whack.
Of course, every drug comes with side effects. Fostamatinib was initially developed to fight auto-immune conditions but can present respiratory problems. “However, the drug was designed for prolonged, continuous use. This is not the case for COVID-19 patients, who only need it for two or three weeks,” Den Dunnen and De Winther told us. They explained that patients taking the drug might experience diarrhoea at worst, which of course means the pros of the drug far outweigh the cons.
Improving patient care together
The Amsterdam-based researchers are also closely linked to the Imperial College London, who are simultaneously carrying out a trial to further understand how this drug can have greater impact. With this recent discovery and knowledge, the research partners can share their data to better understand when to treat patients. By treating them on admission to hospital, doctors can prevent patients going into ICU, explained Den Dunnen and De Winther. If the drug continues to show positive results, this could mean a massive offload of stress for hospital staff, a drastic decrease in ICU admissions, making more room for non-COVID-19 patients and potentially saving many lives.
Watch this video to better understand how the novel coronavirus causes COVID-19.